Monday, July 30, 2007
Illness and the brain
http://www.sciencemuseum.org.uk/exhibitions/brain/22.asp
Your brain
Your brain is the hub of your nervous system. It is made up of 100 billion nerve cells - about the same as the number of trees in the Amazon rainforest. Each cell is connected to around 10,000 others. So the total number of connections in your brain is the same as the number of leaves in the rainforest - about 1000 trillion.
Your nervous system has two parts:
Central nervous system
Your spinal cord receives information from the skin, joints and muscles of your body. It also carries the nerves that control all your movements. Your brain is the most complicated part of your nervous system. It receives information directly from your ears, eyes, nose and mouth, as well as from the rest of your body via the spinal cord. It uses this information to help you react, remember, think and plan, and then sends out the appropriate instructions to your body.
Peripheral nervous system
Some of your peripheral nervous system (PNS) is under your voluntary control - the nerves that carry instructions from your brain to your limbs, for example. As well as controlling your muscles and joints, it sends all the information from your senses back to your brain. Other parts of your PNS are controlled by the brain automatically. This is the autonomic nervous system. It manages some things your body does 'without thinking' like digestion and temperature control.
Senses of how the brain work
In order to keep us alive, the brain uses a set of sensory organs (eyes, ears, nose, tongue, skin) to tell us some of what is going on in the outside world. Remember, we can't hear like a dog, smell like a bear, or see like a hawk. In fact, when compared to the rest of the animal kingdom, human senses seem quite limited.
Our ears hear sound only within a certain range
Our eyes see light in the visual range but not infrared or ultraviolet light
Our perception of touch requires a certain level of pressure
Our sense of smell only helps us if a scent is powerful or nearby
Despite these limitations, our powerful human brains can still integrate the information from all of our different senses and use it to create an internal representation of the external world.
Everything we experience is filtered by our senses. All sensory signals (sound, sight, taste, touch) initiate a cascade of processes in the brain that alter brain structure and function. This process of creating some internal representation of the external world (i.e., information) depends upon the pattern, intensity, and frequency of neuronal activity produced by sensing, processing, and storing signals.
Experience creates a processing template through which all new input is filtered. The more frequently a certain pattern of neural activation occurs, the more indelible the memory becomes. All living organisms have mechanisms to sense and respond to changes in their environments. These mechanisms respond continually and are designed to keep our body's systems in a state of equilibrium or homeostasis.
We have sensory mechanisms to tell the brain what is going on in the internal world of the body. For example, we have special sensory apparatuses that tell the brain the concentration of oxygen in the blood. Other systems sense the concentration of salts (e.g., too much salt causes a sensation of thirst) or gases such as carbon dioxide. These internal sensory mechanisms, like the five senses for the external world, help the brain continuously monitor and act to maintain life.
Process
Once our sensory apparatuses have translated physical or chemical information from the outside (or inside) world into neuronal activity, this set of signals travels up into the brain to be processed. Sensory information from the external environment and the internal environment enters the central nervous system at the level of the brainstem and midbrain.
As this primary sensory input arrives, it is matched against previously stored patterns of activation. If the pattern is unknown, or is associated with previous threat, the brain will activate a set of responses that are designed to help promote survival. (This alarm response is at the heart of the post-traumatic symptoms seen in so many maltreated children.)
http://www.childtraumaacademy.com/amazing_brain/lesson01/page03.html
The Amazing Human Brain and Human Development

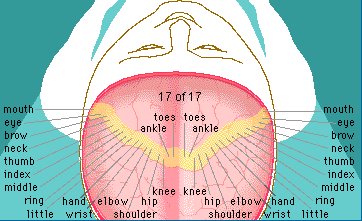
How information enters, and is processed by, your brain. Image courtesy of Bruce D. Perry, M.D., Ph.D.
Saturday, July 28, 2007
Knowledge
http://www.apa.org/topics/topicptsd06b.html
Mind/Body Health: The Effects of Traumatic Stress
People who experience or witness horrible events such as school shootings, combat, rape, torture, natural disasters, accidents or other things in which their physical safety and life -- or the safety and life of others -- was in danger have experienced a traumatic stress. People who are repeatedly exposed to life or death situations, such as EMT and rescue squad workers, police officers, fire fighters and medical personnel on burn wards or trauma units where stress levels and mortality rates are high also witness trauma. Anyone who has experienced these things has experienced a shock and, even if all ultimately escape danger, the people who lived through the event may feel like life “just isn’t the same anymore.” People may experience a variety of reactions, many of which are understandable in the context of experiencing or witnessing traumatic events such as the hurricanes. Experiencing physical or emotional symptoms in response to a traumatic event is normal and is called a traumatic stress reaction.
Physical Symptoms of Traumatic Stress
Anyone affected by the hurricanes or other traumatic stress may experience:
· Fatigue· Being easily startled· Headaches· Sweating· Gastro-intestinal problems
Emotional Symptoms of Traumatic Stress
Those affected by traumatic stress may feel:
· Fear· Anger· Guilt· Anxiety· Reduced awareness· Feeling like you are numb or not part of the world· Helplessness· Hopelessness
What is PTSD?
PTSD stands for Post Traumatic Stress Disorder. This is similar to a stress reaction and, in fact, many people who have experienced a traumatic event do develop PTSD. Those with PTSD may experience many of the same emotional and physical symptoms as those with a traumatic stress reaction. Those with PTSD, however, experience trauma along with intense fear, helplessness or horror and then develop intrusive symptoms (such as flashbacks or nightmares). Their symptoms will last more than a month and get in the way of normal life.
Traumatic stress is not uncommon. In fact:
· About 70 % of U.S. adults have experienced a severe traumatic event at least once in their life and one out of five go on to develop symptoms of PTSD· Approximately 8% of all adults have suffered from PTSD at any one time· If you include children and teens, an estimated 5% of all Americans will develop PTSD during their lifetime or more than 13 million people· About one in 10 women will develop PTSD symptoms during their lifetime or double the rate for men because they are much more likely to be victims of domestic violence, rape or abuse.· Almost 17% of men and 13% of women have experienced more than three traumatic events during their life.
The Mind/Body Connection
Suffering traumatic stress can affect your emotions as well as your body and the two are so connected that it can be hard to tell the difference. For instance, traumatic stress can cause you to lose concentration, forget things, or have trouble sleeping. It may be difficult to determine on your own whether these symptoms are because you do not feel well physically or because you are still upset. Traumatic stress also can lead you to eat in unhealthy ways or to eat foods that are not healthy, and those eating patterns can affect how you sleep or how your stomach feels. Stress can cause headaches, but the pain from the headaches can also make your stress worsen.
Because the body and the mind work in concert, traumatic stress can cause a cycle that makes it seem like the body and mind are working against one another, worsening symptoms like pain and fatigue.
Coping with Traumatic Stress
There are things you can do to help yourself if you have suffered traumatic stress as a result of an event such as a school shooting.
- Give yourself time to heal. Anticipate that this will be a difficult time in your life. Allow yourself to mourn the losses you have experienced. Try to be patient with changes in your emotional state.- Ask for support from people who care about you and who will listen and empathize with your situation. But keep in mind that your typical support system may be weakened if those who are close to you also have experienced or witnessed the trauma.- Communicate your experience in whatever ways feel comfortable to you - such as by talking with family or close friends, or keeping a diary.- Find out about local support groups that often are available such as for those who have suffered from natural disasters. These can be especially helpful for people with limited personal support systems.- Try to find groups led by appropriately trained and experienced professionals such as psychologists. Group discussion can help people realize that other individuals in the same circumstances often have similar reactions and emotions.- Engage in healthy behaviors to enhance your ability to cope with excessive stress. Eat well-balanced meals and get plenty of rest. If you experience ongoing difficulties with sleep, you may be able to find some relief through relaxation techniques. Avoid alcohol and drugs.- Establish or reestablish routines such as eating meals at regular times and following an exercise program. This can be especially important when the normal routines of daily life are disrupted. Even if you are in a shelter and unable to return home, establish routines that can bring comfort. Take some time off from the demands of daily life by pursuing hobbies or other enjoyable activities.--Help those you can. Helping others, even during your own time of distress, can give you a sense of control and can make you feel better about yourself.- Avoid major life decisions such as switching careers or jobs if possible because these activities tend to be highly stressful.
When Should I Seek Professional Help?
Many people are able to cope effectively with the emotional and physical demands brought about by a natural disaster by using their own support systems. It is not unusual, however, to find that serious problems persist and continue to interfere with daily living. For example, some may feel overwhelming nervousness or lingering sadness that adversely affects job performance and interpersonal relationships.
Individuals with prolonged reactions that disrupt their daily functioning should consult with a trained and experienced mental health professional. Psychologists and other appropriate mental health providers help educate people about common responses to extreme stress. These professionals work with individuals affected by trauma to help them find constructive ways of dealing with the emotional impact.
With children, continual and aggressive emotional outbursts, serious problems at school, preoccupation with the traumatic event, continued and extreme withdrawal, and other signs of intense anxiety or emotional difficulties all point to the need for professional assistance. A qualified mental health professional such as a psychologist can help such children and their parents understand and deal with thoughts, feelings and behaviors that result from trauma.
APA is grateful to Paul J. Rosch, M.D.. President, The American Institute of Stress, for his help in developing this fact sheet.
http://www.apahelpcenter.org/articles/article.php?id=122
A new kind of war
BY MARK GREERMonitor StaffPrint version: page 40
In her work with U.S. veterans, psychologist Kaye Baron, PhD, may be seeing the opening salvos of a new war--one for mental health. The private practitioner in Colorado Springs, Colo., near the Fort Carson Army Base, serves a lot of military families affected by U.S. operations in Iraq and Afghanistan. She is also a contract psychologist for a local government agency for which she has evaluated more than 75 military personnel who have returned from Iraq showing depression and irritability and reliving intense emotional trauma--some of the classic signs of post-traumatic stress disorder (PTSD).
"I've seen a lot of PTSD symptoms, if not full-blown PTSD," Baron says. "The social withdrawal, the nightmares, the sleep disturbances, the memory and concentration problems, the anger, the lack of trust--I'm seeing all this within the troops coming back from Iraq."
Baron's contacts through her evaluations and work with military families are among the first of what at least one study says could be many more military personnel returning from Iraq suffering--or who will later suffer--from PTSD. While the majority of troops show resilience from the stresses of war, some do or will need help with PTSD symptoms.
Already, in one recent army report, more than 1,000 troops reported PTSD symptoms--and troops' reluctance to admit problems may mean the real number is higher. In a war characterized by intensely stressful surprise attacks and street fighting, that number may only increase, some psychologists predict. Unfortunately, a lack of research means psychologists are still working to fully understand PTSD.
Service providers have observed what is now known as PTSD for decades. Called anything from operational fatigue to shell shock, the disorder acquired its current name only in 1980, when PTSD was added to the third edition of the Diagnostic and Statistical Manual of Mental Disorders. And research on the early signs and symptoms of combat trauma is scant. Most research on Vietnam War veterans did not take place until 1980s.
Read the rest here
http://www.apa.org/monitor/apr05/war.html
Violence and Risk of PTSD, Major Depression,
Heidi S. Resnick, and Connie L. Best
Medical University of South Carolina
With a national household probability sample of 4,023 telephone-interviewed adolescents ages 12–17,
this study provides prevalence, comorbidity, and risk-factor data for posttraumatic stress disorder
(PTSD), major depressive episode (MDE), and substance abuse/dependence (SA/D). Roughly 16% of
boys and 19% of girls met criteria for at least 1 diagnosis. Six-month PTSD prevalence was 3.7% for boys
and 6.3% for girls, 6-month MDE prevalence was 7.4% for boys and 13.9% for girls, and 12-month SA/D
prevalence was 8.2% for boys and 6.2% for girls. PTSD was more likely to be comorbid than were MDE
and SA/D. Results generally support the hypothesis that exposure to interpersonal violence (i.e., physical
assault, sexual assault, or witnessed violence) increases the risk of these disorders and of diagnostic
comorbidity.
Read the rest here its a pdf file very good research
http://www.apa.org/journals/releases/ccp714692.pdf
CHRONIC EXPOSURE TO STRESS HORMONE CAUSES ANXIOUS BEHAVIOR IN MICE, CONFIRMING THE MECHANISM BY WHICH LONG-TERM STRESS CAN LEAD TO MOOD DISORDERS
WASHINGTON - Neuroscientists at Harvard Medical School and its affiliate McLean Hospital have shown that long-term exposure to stress hormone in mice directly results in the anxiety that often comes with depression. After years of circumstantial evidence linking stress and depression, this evidence may be the "smoking gun" of what, for some, causes some types of mood disorders. The research appears in the April issue of Behavioral Neuroscience, which is published by the American Psychological Association.
The findings are important for understanding the causes and improving the treatment of depression. Scientists already knew that many people with depression have high levels of cortisol, a human stress hormone, but it wasn’t clear whether that was a cause or effect. Now it appears likely that long-term exposure to cortisol actually contributes to the symptoms of depression.
Paul Ardayfio, PhD candidate, and Kwang-Soo Kim, PhD, of the Molecular Neurobiology Laboratory at McLean Hospital, made their discovery by exposing mice to both short-term and long-term durations of stress hormone, which in rodents is corticosterone. In humans, usually ongoing, chronic stress, such as caring for a spouse with dementia, rather than acute stress, has been associated with depression.
Using 58 mice, the researchers gave the hormone in drinking water so as not to confound the results with the stress of injection. Chronic doses were 17 to 18 days of exposure; acute doses were 24 hours of exposure.
Compared with mice given stress hormone for a day, mice given stress hormone for more than two weeks took significantly longer to emerge from a small dark compartment into a brightly lit open field, a common behavioral test of anxiety in animals. In other words, they seemed more fearful and were less willing to explore the new environment. Chronic but not acute treatment also dulled reactions to a startling stimulus, another sign their nervous systems were overwhelmed.
To the best of the authors’ knowledge, this was the first experiment to compare the effects of chronic corticosterone with the effects of acute corticosterone on anxiety-like behavior.
Given four related lines of evidence, the findings were not a complete surprise. First, more than half the people with Cushing’s disease, in which a disordered adrenal system releases too much cortisol, have depression and anxiety. Second, the "anxious-retarded" subtype of depression is commonly associated with disruption of that same hormonal system. Third, people getting corticosteroid therapy for inflammatory and other disorders have increased mood-related side effects, including anxiety and depression. Fourth, higher glucocorticoid levels for chronic periods have been linked to increased activity in anxiety-related brain regions such as the amygdala in both rodents and humans.
Now the pieces fit together around a central axiom: Stress hormone can cause anxiety, which appears with depression. Having found this causal link in a controlled laboratory setting, the authors say, "Our results suggest that chronically high levels of cortisol, which occurs in Cushing’s disease and some subtypes of depression, can increase anxiety on the one hand and dull responses to external stimuli on the other." The difference between the responses to acute and chronic hormone exposure strengthen the view that very-short-term or acute exposure, they add, "may be adaptive, whereas chronic exposure has detrimental effects on brain and behavior."
Ardayfio and Kim say that outlining the relationship between physiological disruptions and subsequent behavior may help researchers to design new psychiatric drugs that treat the causes of disease rather than peripheral disease-related phenomena. The authors speculate that drugs that reverse or block the deleterious effects of chronically elevated stress hormones may help guard against some types of anxiety symptoms in depression, citing preclinical evidence in rats.
Article: "Anxiogenic-like Effect of Chronic Corticosterone in the Light-Dark Emergence Task in Mice," Paul Ardayfio, PhD candidate, and Kwang-Soo Kim, PhD, McLean Hospital and Harvard Medical School; Behavioral Neuroscience, Vol. 120, No. 2.
Full text of the article is available from the APA Public Affairs Office and at http://www.apa.org/journals/releases/bne1202249.pdf
For inquiries, contact Cynthia Lepore at (617) 855-2110 via
email.
Exposure Therapy Helps PTSD Victims Overcome Trauma's
Findings
Posttraumatic stress disorder (PTSD), a debilitating disorder involving intrusive thoughts associated with traumatic events, affects millions of Americans. First known as “shell shock” and seen in WWI veterans, PTSD often involves flashbacks and nightmares following a traumatic experience, including traffic accidents. Many of these symptoms first surface many months after the trauma.
In the 1980’s, Dr. Terence M. Keane and his colleagues found that exposure therapy was effective in treating the PTSD symptoms of Vietnam War veterans. Exposure therapy, previously known as imaginal flooding therapy, involves carefully exposing the patient to prolonged and repeated imagined images of the trauma until the images no longer cause severe anxiety. In Keane’s randomized clinical trial involving 24 Vietnam veterans, Keane found that exposure therapy was effective in reducing many of the veteran’s PTSD symptoms, including nightmares, flashbacks, memory and concentration problems, and irritability.
Exposure therapy doesn’t just help combat veterans with PTSD. Research by Dr. Edna B. Foa and her colleagues showed that exposure therapy was effective in reducing PTSD symptoms of rape victims, including persistent fear. The improvements were seen immediately after exposure therapy, and were shown to be sustained during a three-month follow-up.
Significance
Many American suffer from PTSD. According to the National Institutes of Mental Health, 5.2 million Americans aged 18-54 have PTSD. These and dozens of subsequent studies have established exposure therapy as a highly effective and perhaps the most efficient treatment for PTSD. Research completed after the September 11, 2001 terrorist attacks found an increased prevalence of PTSD, especially in children living in New York City.
http://www.psychologymatters.org/keane.html
Women Are Diagnosed With PTSD More than Men, Even Though They Encounter Fewer Traumatic Events, Says Research
WASHINGTON, DC—Males experience more traumatic events on average than do females, yet females are more likely to meet diagnostic criteria for Posttraumatic Stress Disorder (PTSD), according to a review of 25 years of research reported in the November issue of Psychological Bulletin, published by the American Psychological Association (APA).
The authors reviewed 290 studies conducted between 1980 and 2005 to determine who is more at risk for potentially traumatic events (PTE) and PTSD – males or females? The results of the meta-analysis found that while males have a higher risk for traumatic events, women suffer from higher PTSD rates. PTSD is defined as an anxiety disorder precipitated by a traumatic event and characterized by symptoms of re-experiencing the trauma, avoidance and numbing and hyperarousal.
From the review, researchers David F. Tolin, PhD of the Institute of Living and Edna B. Foa, PhD, of the University of Pennsylvania School of Medicine found that female study participants were more likely than male study participants to have experienced sexual assault and child sexual abuse, but less likely to have experienced accidents, nonsexual assaults, witness death or injury, disaster or fire and combat or war. Sexual trauma, the authors conclude, may cause more emotional suffering and are more likely to contribute to a PTSD diagnosis than other types of trauma.
Women’s higher PTSD rates were not solely attributable to their higher risk for adult sexual assault and child sexual abuse, explained Tolin. PTSD rates were still higher for women even when both sexes were compared on the same type of trauma.
“PTSD may be diagnosed more in women in part because of the criteria used to define it. Cognitive and emotional responses to traumatic events make a diagnosis of PTSD more likely. So even though men may experience more traumas, they don’t seem to have the same emotional responses to traumatic events,” said Tolin and Foa.
Furthermore, according to the authors, those participants who experienced multiple traumas may be more vulnerable to re-experiencing old PTSD symptoms when confronted with a new trauma. For example, if one studies male and female survivors of a motor vehicle accident, typically the female accident victims report more PTSD symptoms than do the male accident victims. “However, the data suggest that the female victims will have brought to the table a much greater risk of abuse and sexual assault prior to the accident; this could place them at higher risk of developing PTSD after the accident even though the current accident may not have caused all the symptoms,” said Tolin.
These findings were consistent regardless of the population and age examined and the type of study and assessment tool used.
A reason that men may not fit the current diagnosable criteria of PTSD, said Tolin, is that their symptoms may manifest themselves differently. The male participants examined in this review were less likely to report anxiety or depression, but were more likely to report behavior and drug problems. They were also more likely to become irritable, angry or violent after traumas.
Understanding that responses to trauma can vary from person to person will help better determine if a person has experienced a trauma, said Tolin. An example of how subjective trauma symptoms can be illustrated in research investigating the traumatic effects of 9/11 terrorist attacks. Quite a few studies showed that participants’ distance from ground zero was directly related to the likelihood of experiencing severe PTSD symptoms. But, said Tolin, “People from all over the U.S. could technically have been classified in research as having ‘experienced’ a terrorist attack just by watching it on TV. This is a major problem for trauma research because it’s hard to determine whether someone has really been traumatized or not.”
“Simple checklists or short interviews are insufficient for assessing trauma and this is what is used most in these types of situations. More thorough assessments are needed to know if someone will suffer long-lasting symptoms from an accident, attack or disaster,” said the authors.
Article: “Sex Differences in Trauma and Posttraumatic Stress Disorder: A Quantitative Review of 25 Years of Research,” David F. Tolin, PhD, Institute of Living and University of Connecticut School of Medicine and Edna B. Foa, PhD, University of Pennsylvania School of Medicine; Psychological Bulletin, Vol. 132, No. 6.
Full text of the article is available from the APA Public Affairs Office and at http://www.apa.org/journals/releases/bul1326959.pdf
Dr. Tolin can be reached by phone at (860) 545-7685 or by
e-mail.
New Insurance Legislation Would End Discrimination Against People With Mental Health Disorders
WASHINGTON, Feb. 12 /PRNewswire-USNewswire/ -- Today, the United States Senate took an important step toward meeting the mental health needs of tens of millions of Americans by introducing new legislation to end discrimination against people with mental health disorders and assure treatment is available for those who need it. The Mental Health Parity Act of 2007, introduced by Sens. Pete Domenici (R-N.M.), Edward Kennedy (D-Mass.) and Michael Enzi (R- Wyo.), would provide mental health insurance coverage equivalent to physical health coverage, benefiting 113 million Americans in large group health plans.
"Having a mental health disorder can be as serious as having a heart attack or any other debilitating, life-threatening physical health disorder. In addition, there is a clear connection between mental health disorders and physical ailments," says Russ Newman, PhD, JD, APA executive director for professional practice. "With the passage of this bill, insurers may no longer arbitrarily limit the number of hospital days or outpatient treatment sessions, or use higher copayments or deductibles for people in need of psychological services."
This new legislation, modeled on the current Federal Employee Health Benefits Program covering 8.5 million federal employees, strengthens provisions in the original Mental Health Parity Act of 1996 and closes loopholes in this law. The 2007 bill requires that copayments for office visits, deductibles, limits on number of visits, out-of-network and in-network services for psychological services be treated the same as physical health services. It also includes coverage for substance abuse and chemical dependency services. In addition, the bill preserves existing state laws requiring diagnoses coverage.
According to APA consumer research, 85 percent of Americans say health insurance should cover mental health services. And 87 percent say it's lack of insurance coverage that most keeps them from seeing a mental health professional.
"Health care coverage in this country needs to catch up with what people increasingly understand...the mind and body are linked inextricably," says Newman. "Congress can help improve access to mental health services and end insurance discrimination against those suffering from mental health disorders by passing the Mental Health Parity Act of 2007."
The American Psychological Association (APA), located in Washington, DC, is the largest scientific and professional organization representing psychology in the United States and is the world's largest association of psychologists. APA's membership includes more than 150,000 researchers, educators, clinicians, consultants and students. Through its 54 divisions and its affiliations with 60 state, territorial and Canadian provincial associations, APA works to advance psychology as a science and profession, and as a means of promoting health, education, and human welfare.
SOURCE: American Psychological Association
CONTACT: Tomeka Rawlings, +1-202-336-5898, trawlings@apa.org, or LuanaBossolo, +1-202-336-5898, lbossolo@apa.org, both of American PsychologicalAssociation
Web site: http://www.apa.org/
Study shows increased amygdala activity in those who were closer to the 9/11 disaster
WASHINGTON, DC—Exposure to trauma may create enough changes in the brain to sensitize people to overreact to an innocuous facial gesture years later, even in people who don’t have a stress-related disorder, says new research. It appears that proximity to high-intensity traumas can have long lasting effects on the brain and behavior of healthy people without causing a current clinical disorder. But these subtle changes could increase susceptibility to mental health problems later on. These findings are reported in the May issue of Emotion, published by the American Psychological Association (APA).
http://apa.org/releases/brain_function.html
Trauma and Resilience Research
Welcome to the center for the study of Trauma and Resilience at Columbia University/New York State Psychiatric Institute
We are a nonprofit academic center specializing in the diagnosis and treatment of Posttraumatic Stress and grief-related problems, and offer effective, specialized treatment that is not widely available elsewhere. Our mission is two-fold: to improve mental health services and extend our knowledge of the psychological impact of traumatic events. Our professionals all hold faculty positions with Columbia University and offer compassionate, expert care at no cost to the client.We invite you to explore our site and learn more about our services, innovative research programs, and faculty.
Thousands of New Yorkers are still struggling from symptoms of Posttraumatic Stress Disorder related to the 9/11 terrorist attacks. People with PTSD routinely struggle with intense anxiety and fear, vivid memories and nightmares, irritability with others, avoidance of places related to 9/11, poor concentration, numbness and depression, and becoming increasingly isolated. They often have great difficulty functioning from day to day, and over time can feel increasingly alone.The good news is that PTSD is a treatable problem, and we have a nationally recognized program that focuses on helping people with PTSD through treatment and treatment research. The goal of all our treatment research is to improve the lives of people with these and similar problems by developing new and better treatments. All treatment is provided at no cost to our clients. If you or someone you know might need help with 9/11-related problems like these, please call us for more information on our research and treatment program.
http://www.columbiatrauma.org/
Summeries of recent research
Following are short descriptions of recent research on posttraumatic stress disorder. Keep in mind that hundreds of articles on PTSD are published each year. The articles listed below are a few that have sparked our interest. We will be adding new research summaries and hope you will revisit our site to learn what is new on PTSD. New research on the treatment of PTSD is in the treatment section of this web site.
Predictors of PTSD and delayed PTSD after disaster: the impact of exposure and psychosocial resources. R.E. Adams and J.A. Boscarino. Journal of Nervous and Mental Diseases, 194:485-493, 2006.
Using survey data from adults who were living in New York City on September 11, 2001, researchers tried to identify factors associated with PTSD. Surveys were conducted one-year and two-years after the World Trade Center Disaster (WTCD). Factors associated with PTSD included being younger, being female, experiencing more WTCD events, experiencing more traumatic events and negative life events other than the WTCD, having low social support and having low self-esteem. Read an abstract of this study.
Posttraumatic stress disorder among military returnees from Afghanistan and Iraq. M.J. Friedman. American Journal of Psychiatry, 163:586-593, 2006.
Although most military personnel returning from Afghanistan and Iraq adjust successfully, a significant number will exhibit PTSD or some other psychiatric disorder. With a focus on war zone trauma, data on prevalence, diagnosis, pathophysiology, and treatment of PTSD is reviewed. Using evidence-based practices, partial improvement can be achieved for most patients and complete remission can be achieved in 30%-50% of PTSD cases
Friday, July 27, 2007
PTSD
Characteristic symptoms may include
persistent re-experiencing of the traumatic event(s).
avoiding experiences or people that trigger memories of such event(s).
increased arousal, to include nervousness, over-reaction to sudden noises, (are you jumpy?), difficulty sleeping (night sweats), and nightmares (ever hit your wife, girlfriend in your sleep, or are they scared to wake you up?).
bouts of "inappropriate" rage and-or depression.
difficulty relating emotionally to others.
feelings of extreme alienation and meaninglessness.
isolation from others (do others see you as cold, unfeeling?).
in the most extreme cases, persistent thoughts of murder and-or suicide.
http://www.bringthemhomenow.org/stand/ptsd.html
This is solider ptsd
This is child trauma ptsd lets see if they are equal
Post-Traumatic Stress Disorder (PTSD)
What is Post-Traumatic Stress Disorder?
Post-Traumatic Stress Disorder, PTSD, is an anxiety disorder that can develop after exposure to a terrifying event or ordeal in which grave physical harm occurred or was threatened. Traumatic events that may trigger PTSD include violent personal assaults, natural or human-caused disasters, accidents, or military combat.
Signs & Symptoms
People with PTSD have persistent frightening thoughts and memories of their ordeal and feel emotionally numb, especially with people they were once close to. They may experience sleep problems, feel detached or numb, or be easily startled.
http://www.nimh.nih.gov/healthinformation/ptsdmenu.cfm
This really brought to light for me how much child trauma affects the human body it is equaled to combat ptsd. You can look really like nothing is wrong on the outside but your insides know, we need to educate people about ptsd so we can all heal soldiers included.
What is Combat PTSD?
Many Vietnam veterans returned home to a troubled period of readjustment from their wartime experiences. Their emotional problems were characterized initially as post-Vietnam syndrome. It took mainstream psychiatry till the mid-1980’s to finally codify symptoms that have been associated with returning combat veterans since time immemorial. What had been dubbed "homesickness" after the Civil War, shell shock in WWI, and combat neurosis during WWII, was finally recognized by the American Psychiatric Association as an anxiety disorder in its own right, and termed post traumatic stress disorder — or PTSD.
http://www.bringthemhomenow.org/stand/ptsd.html
When the service member is diagnosed, she/he should immediately call 1-800-827-1000, and ask to be connected to the Veterans Administration Regional Office
Thursday, July 26, 2007
Traumatic Stress Linked to Health Problems
Traumatic Stress Linked to Health Problems
The link between health problems and children in low income, single-mother families is not surprising; these children are also more apt to be exposed to violence and maltreatment within the community and their families.A study in the March issue of The Journal of Pediatrics examines whether traumatic stress reactions in children due to these adverse childhood experiences also play a role in predicting their health.
Sandra Graham-Bermann, Ph.D. and Julia Seng, Ph.D., CNM, from the University of Michigan interviewed the mothers and teachers of 160 children, ages four through six, recruited from Head Start programs in two Michigan counties.
They found that 65 percent of the children were exposed to at least one incident of violence in their communities, which ranged from less severe (beatings and chasings) to severe (shootings, stabbings, and rapes).
Also, 47 percent were exposed to at least one incident of violence in their families, such as child maltreatment and domestic violence.A total of 90 percent of those exposed to some form of violence had reactions characterized as traumatic stress (i.e. having nightmares, thumb-sucking, or bed-wetting), and 20 percent were at high risk for developing post traumatic stress disorder.
Nearly one-third of the children had allergies, asthma, or attention deficit hyperactivity disorder (ADHD). Children who had one or more of these three health problems were significantly more likely to have been exposed to violence within the family and to have shown signs of traumatic stress.
Substance Abuse Also a FactorChildren with asthma or gastrointestinal problems were almost four times more likely to have post traumatic stress disorder than the children without these health problems.Dr. Graham-Bermann points out that the direction of these effects -- in other words, whether post traumatic stress disorder causes illnesses or illnesses cause post traumatic stress disorder -- is presently unknown. The research also indicated that substance abuse and the overall health of the mother were factors in predicting children's health problems.
While preventing family and community violence may be beyond the control of health care providers, the authors suggest that clinical interventions to increase the mothers' safety and health may improve their ability to protect their children. In addition, health care providers may be able to treat child traumatic stress symptoms or refer children exposed to violence to group or individual therapy, which may improve their health and well-being.
http://crime.about.com/od/childneglect/a/ajm050308.htm
Good Can Come From Evil
From Janet Martin
Good Can Come From Evil
The story of Lattie McGee and Cornelius Abraham is one of almost unbelievable abuse and cruelty, and yet it is also one of courage and hope.
On August 14, 1987, in a hot South Side Chicago apartment, police and paramedics found the tortured body of four-year-old Lattie McGee. Over the summer, when many inner-city children were outside enjoying splashing in the flow of spraying water hydrants, little Lattie was being systematically tortured by his mother and her boyfriend.
The then 28-year-old Alicia Abraham and her 40-year old boyfriend, Johnny Campbell, spent the summer beating the small boy with their fists, burning him with cigarettes and an iron, dunking his small legs into boiling water, depriving him of food and water, sticking him repeatedly with sewing needles and then wrapping a clothing line around his tiny raw ankles and hanging him upside down in the closet for the night.
To muffle the innocent boy's cries, the couple would sometimes stuff a rag in his mouth.
Campbell did not like the 4-year-olds "effeminate" voice so to toughen the young boy he would starve him then beat him if he complained. On the hot August night, Campbell and Alicia stuffed a rag into Lettie's mouth, potato peels were placed on his eyes, his hands were bound, and he was hung by his feet in the closet. His complaints of having problems swallowing and that he was in pain from the broken collarbone and broken pelvis, were ignored.
Flesh Ripped Away The next morning Alicia Abraham seemed more concerned with watching TV then getting Lattie down from the closet. It would not have mattered because he died sometime during the night. There was no more pleasure for her and her boyfriend to get from abusing this innocent child.
Pathologist said Lattie died of a severe blow to the head that slowly killed him, but they added, "His emaciated body, scarred from head to foot, was so infected from untreated wounds that he probably would have died a short time later." When the paramedics and police lifted the boy's shirt, they uncovered a chest of raw skin, his flesh ripped away from repeated abuse.
Not the Only Victim There was another child in the home, six-year-old Cornelius Abraham, Lattie's brother. With courage, the young boy testified against the Alicia and Campbell. He recounted all the episodes of abuse that he and Lattie suffered.
For their crimes, Johnny Campbell and Alicia Abraham were both sentenced to life in prison.
Remarkably, two years earlier in 1985, Alicia Abraham was being counseled for neglecting her children by state investigators, who incredibly concluded the situation had improved.
Out of Despair, Hope Cornelius, who showed much courage, was eventually sent to live with his biological father. Sadly, his father also neglected him, and at age 12, he was homeless and on his own for three months. After five more tumultuous years, Cornelius was placed with a pair of loving foster parents. In time, Cornelius grew close to them and today calls them "Mom and Dad."
After graduating from high school, he went on to college. In 1999, the YMCA Network for Counseling and Youth Development of Greater Chicagoland presented Cornelius with the first ever, Cornelius S. Abraham Award, designed to give hope to children who have suffered from abuse.
As summer ends, I cannot help to think of Lettie, who would be 20 years old now. Since I first read the Abraham brothers' story of the monstrous cruelty at the hands of their caregivers, I think of Lettie at summer's end. I will never understand what makes people, such as Alicia and Campbell, do the horrific cruel acts to small children, and in a way, I hope I never do understand it. Then I refocus and think of Cornelius -- so brave, so determined to beat the odds -- and I send a silent wish to him: that his life is now one of peace and happiness.
Janet Martin, the writer of this article, is a frequent visitor to the About Crime & Punishment site, and lives in the Chicago area.
http://crime.about.com/od/v_childabuse/a/uc_lettie.htm
A story of my own
Wednesday, July 25, 2007
2001 Total Daily Cost of Child Abuse & Neglect in the United States
Direct Costs Estimated Daily Cost
Health Care System
Hospitalization $17,001,082
Chronic Health Problems $8,186,185
Mental Health Care System $1,164,686
Child Welfare System $39,452,054
Law Enforcement $67,698
Judicial System $934,725
Total Direct Costs $66,806,430
Indirect Costs
Special Education $612,624
Mental Health and Health Care $12,678,455
Juvenile Delinquency $24,124,086
Lost Productivity to Society $1,797,260
Total Indirect Costs $190,938,452
TOTAL COSTS $257,744,882
http://www.preventchildabusega.org/pdf/secure-charteredcouncil/Cost.of.child.abuse.pdf
What can you do if you believe a child is being abused or neglected?
Report, report, report. Everyone has the right and responsibility to report any incidence of suspected child abuse at any time. Actual knowledge of abuse is not required; all you need is “reasonable cause, suspicion, or belief” based on your observations. Information to support your concern may include your firsthand observations or beliefs, your professional training or experience, or statements made by the child or parent.
Having only limited information about your suspicion should not prevent you from making a report. Remember, you do not have to be “right” in your suspicions; you simply need to have a heightened and rational concern for the safety and well-being of a child.
Also, all states have laws that protect reporters from legal liability as long as reports are made in “good faith.”
http://crime.about.com/gi/dynamic/offsite.htm?zi=1/XJ/Ya&sdn=crime&cdn=newsissues&tm=4594&gps=210_383_1020_619&f=20&tt=14&bt=1&bts=1&zu=http%3A//www.americanhumane.org/site/PageServer%3Fpagename%3Dlk_resource_center
You Carry the Cure In Your Own Heart
by Andrew VachssOriginally published in Parade Magazine, August 28, 1994
http://www.vachss.com/av_dispatches/disp_9408_a.html
Monday, July 23, 2007
Addictive behaviors where do they come from
.com/evolution/brainabuse.html
Sunday, July 22, 2007
Hotline Numbers
If your in need of help please contact someone to help you
Saturday, July 21, 2007
Friday, July 20, 2007
Thursday, July 19, 2007
How your Brain responds to stress
http://www.fi.edu/brain/stress.htm
Wednesday, July 18, 2007
The simple explanation of what leads to PTSD
http://www.agsp.de/html/a20.html
Amygdala
Sunday, July 15, 2007
It is important to understand that the abused child’s reaction to stress is not abnormal
The experience of moderate and predictable stress in childhood has not been found to be particularly harmful – in fact this low level of stress can help children to develop ways of coping with life in general. However, chronic stress sensitises neural pathways and overdevelops the regions of the brain that deal with anxiety and fear responses.
Children who are constantly under threat of abuse will need to focus their brain’s resources on survival and responding to threats in their environment. The chronic stimulation of fear responses hinders the stimulation of parts of the brain involved in more complex thought and this effects learning.
Cortisol is a hormone that helps the body prepare to cope with stress, and studies have shown that children who have been subjected to abuse have abnormal secretions of cortisol (Hart, Gunner, Cicchetti, 1995).
It is important to understand that the abused child’s reaction to stress is not abnormal: their brain development is often an adaptive response to their negative environment. However, it is maladaptive to other environments. If the brain’s main focus is survival it will be more difficult to develop healthy cognitive and social skills. Abused children often have great difficulty when presented with kindness, nurturing and stimulation: their brains may have underdeveloped pathways to adapt to this new world.
Repeated abuse and resulting stress may cause an affect on the neurochemical systems which can cause changes in: attention, impulse control, sleep patterns, and fine motor control (Perry 2000).
http://www.teachingexpertise.com/articles/child-abuse-and-its-effect-on-brain-development-1448
How trauma affects the brain
As well as emotion, the limbic brain is important in the area of memory and smell, which are also important in the flight or fight response.
Any lesion to the hippocampus (from trauma) results in loss of memory for up to a month. Therefore, it is important to intervene immediately to assist victims of trauma before trauma is recorded in the long-term storage area called the cerebral cortex (the outside covering of the brain).
Case Study: In a study conducted by Bremner and his research team, it was shown that atrophy and dysfunction of the hippocampus in PTSD leads to distortions and fragmentation of memories e.g. a girl who was constantly locked in a closet, remembered the smell of old clothes but had no visual memory of being in the closet. With the help of psychotherapy and medication, she was able to integrate other aspects of the event into her memory.
Whenever the neurotransmitters are stimulated, the symptoms of PTSD increase. These include: flashbacks, hypervigilance, excessive arousal and increased startle response. (Southwick, S.M. and others,1997). This is also the underlying cause of lack of concentration, being fearful (when there is really nothing to worry about), panic attacks and sleep disturbance. This response also explains why so many PTSD victims use heroin, alcohol etc. to decrease the activity of chemicals in the brain. Southwick’s research showed that as the symptoms of PTSD increased, so did the use of addictions.
http://www.asca.org.au/childabuse/ca_traumaaffectsbrain.html
Friday, July 13, 2007
Tuesday, July 10, 2007
Fibromyalgia Findings
http://www.neurotherapycenters.com/articles/Esty-FF2003.htm
Pathophysiology
The immediate physiologic response to trauma can be significant and may set the stage for lasting PTSD symptoms. Alterations in the noradrenergic and dopaminergic neurotransmitter systems and the stress response of the hypothalamic-pituitary-adrenal axis are well documented in PTSD. Some evidence suggests that chronic PTSD, perhaps through these physiologic changes, can lead to changes in brain microarchitecture.
http://www.emedicine.com/PED/topic2650.htm
Wednesday, July 4, 2007
Neurotherapeutic Treatment of Fibromyalgia
http://www.neurotherapycenters.com/articles/Esty-FF2003.htm
An Overview of Traumatic Attachments and Brain Development
Women Stats
http://www.lawandpsychiatry.com/html/hippocampus.htm
The Lasting Effects of Psychological Trauma on Memory and the Hippocampus
Describe research findings showing reduction in volume of the hippocampus in posttraumatic stress disorder related to abuse or combat andtheoretical explanations for findings
Describe how dysfunction of medial prefrontal cortex may contribute to symptoms of stress-related disorders like PTSD.
http://www.lawandpsychiatry.com/html/hippocampus.htm
Stress and its Effect on the Brain
A study, reported in The American Journal of Psychiatry in 1995, was lead by Dr. Douglas Bremner and Dr. Dennis Charney at the Veterans Affairs Medical Center in West Haven, showed a physical alteration, an 8% reduction in the volume of the right hippocampus compared with those who suffered no symptoms. In addition, the study showed survivors of childhood abuse performed at levels averaging 40% lower on a test of verbal memory than did people of comparable age and education.
Dr. Bremner said, "the memory of those with post-traumatic symptoms is particularly faulty for words, like grocery lists or phone numbers. The study found no deficiency in the trauma victim's overall IQ scores, however."
The shrinkage of the hippocampus may be due to the effects of heightened levels of cortisol, a steroid hormone secreted by the brain in response to emergencies. Dr. Bremner said "Cortisol can be toxic to the hippocampus." Yet, there were conflicting reports in which cortisol was also shown to be at low levels in concentration camp post-traumatic survivors. "There are mixed findings on cortisol levels in trauma victims. . . biologically speaking, there may be different kinds of post-traumatic stress."
http://www.brainchannels.com/evolution/brainabuse.html
Sunday, July 1, 2007
Child Abuse and the Brain
There's no doubt that child abuse has serious consequences. The effects, however, may be even worse than you think. An increasing amount of research indicates that severe maltreatment at an early age can create an enduring negative influence on a child's developing brain. The findings highlight the seriousness of childhood abuse and may lead to increased prevention efforts as well as new approaches for treatment.
A twisted arm. No food. Rape. It's heartbreaking to think about. Almost 900,000 children faced some form of abuse or neglect in 2000, according to the most recent data from the U.S. Department of Health and Human Services. Clearly these actions have serious consequences, but the extent and nature of the effects were unclear. Now, an increasing amount of research indicates, that while physical wounds often heal over time, severe maltreatment at an early age can create an enduring, harmful influence on a child's developing brain. The research is leading to:
A better understanding of how negative environments affect the brain.
Increased efforts to intervene and protect children from maltreatment.
New ways to treat abuse.
As children sprout in stature over the years, so do their brains. The cells and circuits build and refine. Researchers recently began to suspect that maltreatment might throw a stick in the gear of this sensitive time of growth and cause problems. Although still in an early stage, when looked at altogether, several lines of study support this theory.
For starters, evidence indicates that many maltreated children end up with mental ailments. They appear more likely than healthy individuals to experience learning problems, depression and post-traumatic stress disorder (PTSD), a condition marked by intense anxiety that sometimes erupts after a horrific experience, according to some studies.
Maltreatment also may affect brain anatomy. Compared with healthy individuals who never experienced abuse, some brain areas are smaller in those who experienced maltreatment and have PTSD (see illustration). It's possible that maltreated kids are born with the smaller structures, but many scientists suspect that the finding signals that abuse harms brain development. And these developmental issues may help spur the disorders common in abused and neglected children.
At the root of these problems may be the stress associated with maltreatment. When we experience a stressful situation, our brain's stress system activates a slew of biological actions. This helpful response prepares our body to fight or flee. However, perpetual or intense stress, especially during the brain's sensitive development time in childhood, may harm this system.
In fact, research that measures various stress molecules finds that sometimes they are out of whack in maltreated children and adult survivors. In another example, young rodents separated from their moms for a few hours each day, a source of significant stress, show signs that as adults their stress system does not work properly.
The altered stress system may trigger other problems. Extremely stressful situations appear to cause brain cell death in rodents and may do so in humans as well. In addition, infant monkeys raised individually have a smaller corpus callosum. This collection of fibers that connects the two halves of the brain also was found to be smaller in some maltreated children.
Recently researchers discovered a group of monkeys that will help them better test the effects of stress in child abuse. The mothers naturally act abusive to their offspring. Early findings indicate that the bad parenting alters the stress systems of the abused. Plans to examine brain anatomy are under way.
On the positive side, researchers also are examining maltreated children who do not seem to suffer from mental ailments and function fine in life. They want to know if a person's genetic makeup, a teacher's support or other factors could play a role.
In addition, investigators are testing ways to block or reverse abuse-related biological alterations. For example, early findings indicate that some medications used for depression can reverse problems with the stress system in rats raised in stressful environments and may aid abused children.
Of course, researchers say that the best solution is to prevent maltreatment from occurring in the first place.
Some research shows that maltreatment may affect brain anatomy. For example, in one study researchers examined the brains of maltreated children and adolescents with PTSD. Compared with healthy individuals who never experienced abuse, those who were maltreated have smaller brain areas. Included is the cerebral cortex and prefrontal cortex, which help carry out complex actions; the corpus callosum, which helps the two sides of the brain communicate; as well as the temporal lobes and the amygdala, areas thought to be involved with emotion and memory. Research also finds that a memory area, the hippocampus, is smaller in adult survivors of abuse with PTSD. Although still under investigation, it's possible that experiencing maltreatment during youth harms overall brain development and helps spur the ailments that seem to be common in these individuals.
Illustration by Lydia Kibiuk, copyright © 2003 Lydia Kibiuk.
Can you see where child abuse trauma tunrs into PTSD
Science Daily — Children who were taught a curriculum that focused on self-control and awareness of their own and others’ emotions were found to exhibit greater social competence and fewer behavioral and emotional problems.
According to a recent study in Annals of the New York Academy of Sciences, when teachers taught a particular curriculum to students for 20-30 minutes-per-day, three times-per-week over a six-month period, lower rates of aggression and anxiety/sadness were seen when evaluated a year later compared to children randomized to normal classroom procedures.
“Several complex cognitive processes, such as the ability to cope in stressful situations, are related to the development of the prefrontal areas of the brain starting in the preschool years,” says study author Mark Greenberg. “We know that deficiencies in the function of these lobes are linked to problems like aggression, depression and attention disorders.” Therefore, the Promoting Alternative Thinking Strategies (PATHS) curriculum, which stimulates cognitive and emotional skills, enhances the child’s ability to cope with stress and make good choices.
Greenberg offers an example of a simple PATHS skill that helps children understand and identify feelings in others. “Children use ‘feeling faces’ cards throughout the day to indicate clearly to others what emotions they are experiencing,” says Greenberg. “By labeling the emotions clearly, children learn to recognize them in themselves and others, which will aid them in managing those emotions.”
The main advantage of this curriculum is its preventive nature. Rather than focusing on treating negative behaviors after they have become stable and disruptive, PATHS provides children with coping strategies to prevent the development of behavioral and emotional difficulties.
Note: This story has been adapted from a news release issued by Blackwell Publishing Ltd..
AMYGDALA
Brain. 1. An almond-shaped neuro structure involved in producing and responding to nonverbal signs of anger, avoidance, defensiveness, and fear. 2. A small mass of gray matter that inspires aversive cues, such as the freeze reaction, sweaty palms, and the tense-mouth display. 3. A primeval arousal center, originating in early fishes, which is central to the expression of negative emotions in man.
Usage: Many gestures reflect the amygdala's turmoil. In an anxious meeting, e.g., we may unconsciously flex our arms, lean away, or angle away from colleagues who upset us. Lip, neck, and shoulder muscles may tense as the amygdala activates brain-stem circuits designed to produce protective facial expressions (see, e.g., TENSE-MOUTH) and protective postures (see, e.g., BOW and CROUCH). The amygdala also prompts releases of adrenaline and other hormones into the blood stream, thus stepping-up an avoider's response and disrupting the control of rational thought.
RESEARCH REPORTS: 1. "The amygdala coordinates the actions of the autonomic and endocrine systems and is involved in emotions" (Kelly and Dodd 1991:277). 2. The amygdala may be part of a "general-purpose defense response control network" (LeDoux 1996:158). 3. "Unpleasant odours . . . activate the amygdala and the cortex in the temporal lobe (insula)" (Carter 1998:114).
Neuro notes. In addition to its other duties, the amygdala's gray matter evolved to mediate the evolutionary ancient chemical nervous system, represented today by our bloodstream. Working through the hypothalamus, the amygdala releases excitatory hormones into circulating blood. After surgical removal of the amygdala, growls, screams, angry voices, and other negative signs may lose their meaning and become incomprehensible as afferent cues.
See also AQUATIC BRAIN & SPINAL CORD, CINGULATE GYRUS.
Copyright © 1998 - 2005 (David B. Givens/Center for Nonverbal Studies)Detail of illustration from Mapping the Mind (copyright Weidenfeld & Nicolson 1998)
How the Right and Left Brain work
An inventory of the different ways the right brain and left brain process information. While we have a natural tendency towards one way of thinking, the two sides of our brain work together in our everyday lives. The right brain of the brain focuses on the visual, and processes information in an intuitive and simultaneous way, looking first at the whole picture then the details. The focus of the left brain is verbal, processing information in an analytical and sequential way, looking first at the pieces then putting them together to get the whole.
Left Brain Inventory
• Verbal, focusing on words, symbols, numbers
• Analytical, led by logic
• Process ideas sequentially, step by step
• Make logical deductions from information
• Work up to the whole step by step, focusing on details, information organised
• Like making lists and planning
• Likely to follow rules without questioning them
• Good at keeping track of time
• Spelling and mathematical formula easily memorised
• Enjoy observing
• Plan ahead
• Likely read an instruction manual before trying
Right Brain Inventory
• Visual, focusing on images, patterns
• Intuitive, led by feelings
• Process ideas simultaneously
• 'Mind photos' used to remember things, writing things down or illustrating them helps you remember Words used to remember things, remember names rather than faces
• Make lateral connections from information
• See the whole first, then the details
• Organisation ends to be lacking
• Highly organised
• Free association
• Like to know why you're doing something or why rules exist (reasons)
• No sense of time
• May have trouble with spelling and finding
• Enjoy touching and feeling actual objects (sensory input)
• Trouble prioritising, so often late, impulsive
• Unlikely to read instruction manual before trying
• Listen to how something is being said
• Listen to what is being said
• Talk with your hands
• Rarely use gestures when talking
• Likely to think you're naturally creative, but need to apply yourself to develop your potential
• Likely to believe you're not creative, need to be willing to try and take risks to develop your potential

http://www.windyweb.com/stop.htm