Thursday, November 29, 2007
Whole living body + soul
http://www.marthastewart.com/bodyandsoulmag/
Thursday, November 1, 2007
New Ways to heal pain
Seeing With New Eyes
"The journey of discovery consists not in seeking new landscapes, it is in seeing with new eyes." - Marcel Proust
When you change the way you look at things,the things you look at change.
"In curing, we are looking for answers. In healing, we live questions. In healing, we hang out in the unknown. In healing we trust the emergence of whatever will be, we trust the insight will come. The challenge in medicine is not the choice between one and the other... We need both."
Dr. Paul EpsteinSpirituality and Health Magazine, May / June 2007 Featured article: "The Journey of Naturopath Paul Epstein"
http://www.drpaulepstein.com/
Thursday, September 27, 2007
Invisable Scars
A middle-aged woman walked into my office, took a seat and asked, "Is it possible for me to have been a victim of child abuse if I was never beaten or molested? I responded, "yes" and asked why she asked. She described herself as being frequently depressed and unable to feel good about herself. She said that she felt that she did not know who she was, or what her purpose in life was. She said that her parents were good, strict parents and that, in all honesty, she had no right to feel badly about herself. "After all," she added, "worse things have happened to other people."
I thought that there had to be a reason for her asking her original question even though she insisted that she had a wonderful upbringing. I asked her what her parents' attitude had been like towards her. She said that in her home children were "seen and not heard." She recalled being the "good girl" in the family who always followed the rules. When I asked her what happened if she didn't follow the rules, she said that she never dared rebel but that she often saw her siblings publicly humiliated; they were frequently called "imbecile," "dummy," or "useless." She said that it made her feel afraid, even when she was not the one in trouble. When I asked her what she thought of this tactic, she stated that she knew that her parents did the best that they could. She said that her parents were simply trying to teach all the children the "ways of right and wrong" so that they would grow up to be "disciplined and successful adults." When I asked her if she felt angry about how she and her siblings were treated, she replied, "No, we weren't really allowed to get angry. Anger just makes things worse. Besides, I've always been much too sensitive about things."
It seemed to me that as the "good girl" she even felt guilty questioning her parents as she spoke to me. She spoke in a polite, soft tone, qualified nearly everything that she said, and reminded me several times about her parents' good intentions. When I gently suggested that it may be beneficial that she try to begin to look more at her past and how it may be keeping her from fulfilling her dreams in the present, she said that she was wrong for having come in and that blaming her parents was an ungrateful and disrespectful act. I explained that the goal of therapy is to understand what happened so that she could be as accepting of herself as she was of others. Therapy is never about blame. It's about understanding, healing and growing. This example illustrates one way in which psychological maltreatment had adversely impacted the life of a woman. There are many types of psychological maltreatment and just as many ways that it impacts the emotional, social, and intellectual development of individuals. In this case, although her parents had, perhaps, acted in ways that they felt would be in the best interest of their children, this woman had learned how to "be good" at the expense of learning who she was, what she wanted, and how to express her own feelings. Maybe she was depressed because she was too afraid to take chances and risk making an error; after all, in her family, making an error meant taking the chance of being devastated by humiliation and ridicule.
What is particularly insidious about this form of abuse is that the child victim and the adult survivor often have no idea "what hit them." There are no memories and no physical evidence of being beaten, molested, or abused because the bruises and scars are invisible. It is the soul that is injured.
Part of being a child is to naturally trust one's parents or caretakers and assume that if the adult says, "this is for your own good," it truly is. Even as adults, therefore, victims of psychological maltreatment often find it difficult to trust their own judgment since an integral part of the abuse was reinforcing that they didn't know what was best for them. Many children and adults simply accept the blame and think that they are the problem and are crazy, bad, or worthless. They discredit their own reactions and feelings so that their perceptions match what they are told to think or feel. They often conclude that had they been better, smarter, or more obedient, their parents would have been more loving, supportive, or proud of them. Unfortunately, depression and low self esteem are natural consequences of this process. The good news is: this is treatable. Therapy can bring relief and a new sense of purpose.
http://www.yesican.org/articles/article1-1.html
Tuesday, September 25, 2007
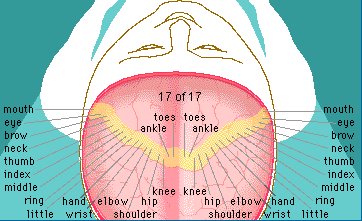
Trauma's Interaction With The Brain
http://www.ptsdforum.org/thread576.html
Conceptualising PTSD - Trauma Response to Anger
Definitions
Amygdala - The brains emotional computer and alarm system
Hippocampus - Brains storage for our most recent concious memories
Thalamus - Translates sights, sounds, smells into the language of the brain
http://www.ptsdforum.org/thread535.html
Little Rock, 50 Years Later and PTSD is present

No black child got in on the appointed day. Three weeks later, armed with a judge's order prohibiting Faubus from interfering, the students were spirited in through a side door (the mob was so unruly, however, police decided the Nine could not stay). In the weeks that followed, they endured unrelenting abuse. They never believed the task would be easy, but they had no idea how hellish it would become. Minnijean Brown Trickey was expelled for a fight she didn't start. "If we knew what it was going to be, we would have been too scared to go," says Trickey, who returned to Little Rock after many years away to care for an aged parent. Decades later, Eckford realized she suffered from posttraumatic stress disorder. For years, she could not work. In her current job since 1999, she has found a measure of peace: it has taken "a long time getting there, a long time to talk about the past without crying."
Charles Ommanney / Getty Images for Newsweek
Now and Then: Eckford today, at her former high school
Mostly, the Nine have flourished. Many got advanced degrees. All moved away—for a while, at least—and Little Rock tried to move on. Mayor Mark Stodola says it's time to put the past aside. He says Little Rock never deserved its racist reputation and that "the people who want to continue to look to the past are an impediment to where we want to go for the future." Ralph Brodie, a Central High football player and student-body president at the time of the crisis, says the reputations of many were unfairly tarnished by the actions of a few. Most people at Central were receptive to the black enrollees, he says, yet the world focused on "problem students—25 maybe, a minuscule percentage." The rest "did everything they could to make that schoolyear work," says Brodie, a lawyer and member of Central's 50th Anniversary Commission.
Monday, September 24, 2007
Healing Veterans with PTSD
PTSD: Regenerative Nutrition Should Help Vets
PTSD: Regenerative Nutrition Should Help VetsBy Dr. Phillip Leveque Salem-News.comPhillip Leveque is a Combat Infantryman, Physician and Nutrition Biochemist.(MOLALLA, Ore.)- Veterans are injured, the VA is broken, and it is time for someone to step up to fix this problem. Many, including myself, talk about how medical marijuana helps veterans with PTSD. Regenerative nutrition can help anyone with PTSD, whether they use medical marijuana or not.The Veteran's Administration (VA) is not staffed to handle the influx of PTSD veterans. Veterans with Post Traumatic Stress Disorder (PTSD) are not receiving proper care or respect. Most do not seek treatment and those that do are often stigmatized and given ineffective prescriptions that erode their quality of life. Let's give them something that may actually work, now. Regenerative Nutrition helps all parts of the body repair and should help the body repair the neurological damage of PTSD. We are assembling a pilot study to examine the impact of a regenerative nutrition product in people with PTSD. This cell renewal beverage from a high-end biotech company has been found to improve mental clarity, focus, vital energy, stress management, and cognitive function in the general population. If the average person is aided by this beverage, imagine how much of a difference it could make in the lives of people with PTSD. This study will enable us to raise public awareness of something that could truly improve the quality of life in veterans with PTSD.According to the Veteran's Administration website, 8% of the population will have PTSD at some time in their lives and 5.2 million Americans each year suffer from PTSD. The VA reports that PTSD affects 30% of Vietnam veterans, 10% of Desert Storm veterans, 6-11% of veterans from Afghanistan, and 12-20% of veterans from the Iraq war. USA Today reported on February 28, 2005, "Of the 244,054 veterans of Iraq and Afghanistan already discharged from service, 12,422 have been in VA counseling centers for readjustment problems and symptoms associated with PTSD." The real numbers today are probably much higher.A 2004 study in the New England Journal of Medicine examining veterans from the current combat operations in Afghanistan and Iraq found that only 23-40% of veterans and military personnel with PTSD sought treatment for the condition. Many veterans fear stigmatization and are concerned about other barriers and/or ineffective care.PTSD has not been treated very effectively with western medicine. Clinics have tried every anti-psychotic and anti-depressant in the book as well as highly potent pain killers like Oxycontin and Morphine with minimal success for PTSD. They did end up with thousands of drug addicts and alcoholics. Veterans are suffering. Rates of suicide and depression among army personnel reached a 26-year high last year, according to the recently released 2006 Army Suicide Event Report. Improvements to the treatment of PTSD could vastly benefit those afflicted, their families, and a society that has been charged with their care.People with PTSD need to repair their damaged nervous systems to be able to heal. The cell renewal beverage is made from nature's pharmacy and is safer than the food we eat. Unlike dangerous pharmaceutical drugs which merely mask symptoms, this beverage could go to the root of the problem, by helping the body repair damage to the brain. We should not let people with PTSD or their families continue to suffer. We need a solution for PTSD. This cell renewal beverage can't hurt, but it could make all the difference in the world for people with PTSD. The VA doesn't have an answer, but perhaps we do. Please help us make a difference: Join our study and help us to take action now. Visit our PTSD Study page at www.LifestyleOregon.com and email health@LifestyleOregon.com to get involved.
Saturday, September 22, 2007
A Soldier's Mind
http://soldiersmind.com/2007/09/20/panel-urges-that-iraqafghanistan-vets-with-ptsd-should-get-lifelong-care/
Resource Networking Research List
Soldiers the places listed below accept your military ChampVA insurance.
Counseling for Individuals, Couples, and Families
Founded in 1974, The Counseling Center in the Berkshires is a private, non-profit pastoral counseling center in Western Massachusetts. CCB is unique in its willingness to blend psychology and spirituality in the process of psychotherapy. All therapists are licensed. All insurances and HMO plans are accepted.
Pittsfield, Williamstown, andGreat Barrington, Massachusetts 413-499-4090
The Counseling Center in the Berkshires, Inc.
Offices:34 Depot Street, Suite 201 . Pittsfield, Massachusetts 01201 . 413-499-4090906 Main Street . Williamstown, Massachusetts 01267 . 413-458-3279 352 Main Street . Great Barrington, Massachusetts 01230 . 413-429-6612
Roberta Russell, Social Worker
Aaron Sardell, Psychologist, Co-Director
Kathryn Jensen, Psychologist, Co-Director
John F. Messerschmitt, Psychologist
Craig G. Clemow, Psychologist
Patricia A. Wallender, Social Worker
Ellen Weiden LCSW
--Behavioral Health Professionals/ Licensed Clinical Social Worker Child or Adolescent Therapy and soldier PTSD.
54 Wendell Ave. Pittsfield Ma. 01201
413-443-1590
Harold Schrager LCSW-
276 South Street STE 3 Pittsfield Ma. 01201
Behavioral Health Professionals/ Licensed Clinical Social Worker Child or Adolescent Therapy and soldier PTSD.
Hilltown Community Centers 58 Old North Road. Worthington Ma. 01098
413-238-5511
Takes all but prime insurance for soldiers and has free care access for filling out the paperwork. The have many programs so if you’re in need check them out.
PTSD Unit at VA. Hospital in Northampton Ma. Director is John
413-582-3053
You can also search the internet for Berkshire county mental health services and find a source that accepts the insurance plan you have.
Crisis Numbers in your time of need.
Telephone: (303) 839-1852 National Council on Child Abuse and Family ViolenceTelephone: toll-free (800) 422-4453 National Coalition Against Domestic Violence
Toll-free (800) 222-2000 National Victim Center CALL - THE VAPTSD Information Line at (802) 296-6300
Friday, September 21, 2007
Invited to a Peace Festival

Tuesday, September 18, 2007
Adrenaline
Contents[hide]
1 History
2 Actions in the body
3 Biosynthesis
4 Regulation
5 Pharmacology
6 Terminology
7 Isomers
8 Autoinjectors
9 See also
10 References
//
[edit] History
In May 1886, William Bates reported the discovery of a substance produced by the adrenal gland in the New York Medical Journal. Epinephrine was isolated and identified in 1895 by Napoleon Cybulski, a Polish physiologist. The discovery was repeated in 1897 by John Jacob Abel.[1]
Jokichi Takamine, a Japanese chemist, independently discovered the same hormone in 1900.[2][3]
It was first artificially synthesized in 1904 by Friedrich Stolz.
[edit] Actions in the body
Epinephrine is a "fight or flight" hormone which is released from the adrenal glands when danger threatens or in an emergency. When secreted into the bloodstream, it rapidly prepares the body for action in emergency situations. The hormone boosts the supply of oxygen and glucose to the brain and muscles, while suppressing other non-emergency bodily processes (digestion in particular).
Epinephrine plays a central role in the short-term stress reaction—the physiological response to threatening, exciting, or environmental stressor conditions such as high noise levels or bright light (see Fight-or-flight response). It is secreted by the adrenal medulla. When released into the bloodstream, epinephrine binds to multiple receptors and has numerous effects throughout the body. It increases heart rate and stroke volume, dilates the pupils, and constricts arterioles in the skin and gut while dilating arterioles in leg muscles. It elevates the blood sugar level by increasing catalysis of glycogen to glucose in the liver, and at the same time begins the breakdown of lipids in fat cells. Like some other stress hormones, epinephrine has a suppressive effect on the immune system.[4]
Although epinephrine does not have any psychoactive effects, stress or arousal also releases norepinephrine in the brain. Norepinephrine has similar actions in the body, but is also psychoactive
http://en.wikipedia.org/wiki/Adrenaline
Cortisol and Stress: How to Stay Healthy
About.com Health's Disease and Condition content is reviewed by our Medical Review Board
Cortisol and Your Body
Cortisol is an important hormone in the body, secreted by the adrenal glands and involved in the following functions and more:
Proper glucose metabolism
Regulation of blood pressure
Insulin release for blood sugar maintanence
Immune function
Inflammatory response
Normally, it’s present in the body at higher levels in the morning, and at its lowest at night. Although stress isn’t the only reason that cortisol is secreted into the bloodstream, it has been termed “the stress hormone” because it’s also secreted in higher levels during the body’s ‘fight or flight’ response to stress, and is responsible for several stress-related changes in the body.
zSB(3,3)
Sponsored Links
CortisolWhat is it? Find out more about this Stress Hormone & it's effects.www.SkinnyOnDiets.com
Weight Loss TipsHealthy weight Loss Get in shape naturallywww.lookcut.com
Cortitrol™ Stress ControlReduce Stress with Cortitrol Stress Control. Balances Cortisol levels.www.PharmanexUSA.comSmall increases of cortisol have some positive effects:
A quick burst of energy for survival reasons
Heightened memory functions
A burst of increased immunity
Lower sensitivity to pain
Helps maintain homeostasis in the body
While cortisol is an important and helpful part of the body’s response to stress, it’s important that the body’s relaxation response to be activated so the body’s functions can return to normal. Unfortunately, in our current high-stress culture, the body’s stress response is activated so often that functioning often doesn’t have a chance to return to normal, producing chronic stress.
Higher and more prolonged levels of cortisol in the bloodstream (like those associated with chronic stress) have been shown to have negative effects, such as:
Impaired cognitive performance
Suppressed thyroid function
Blood sugar imbalances such as hyperglycemia
Decreased bone density
Decrease in muscle tissue
Higher blood pressure
Lowered immunity and inflammatory responses in the body, as well as other health consequences
Increased abdominal fat, which is associated with a greater amount of health problems than fat deposited in other areas of the body. Some of the health problems associated with increased stomach fat are heart attacks, strokes, the development of , higher levels of “bad” cholesterol (LDL) and lower levels of “good” cholesterol (HDL), which can lead to other health problems!
To keep cortisol levels healthy and under control, the body’s relaxation response should be activated after the fight or flight response occurs. You can learn to relax your body with various stress management techniques, and you can make lifestyle changes in order to keep your body from reacting to stress in the first place. The following have been found by many to be very helpful in relaxing the body and mind, aiding the body in maintaining healthy cortisol levels:
Guided Imagery
Journaling
Self-Hypnosis
Exercise
Yoga
Listening to Music
Breathing Exercises
Meditation
Sex
Other Techniques
Cortisol secretion varies among individuals. People are biologically ‘wired’ to react differently to stress. One person may secrete higher levels of cortisol than another in the same situation. Studies have also shown that people who secrete higher levels of cortisol in response to stress also tend to eat more food, and food that is higher in carbohydrates than people who secrete less cortisol. If you’re more sensitive to stress, it’s especially important for you to learn stress management techniques and maintain a low-stress lifestyle.
http://stress.about.com/od/stresshealth/a/cortisol.htm
Monday, September 17, 2007
There's a Lil Girl Inside
There's a lil girl in side, Wanting to get out. She's so tired of the tears, So tired of the fears, And so tired of the pain. Why can't it all just go away? She feels so trapped inside. Screaming and feeling the need to get out. She feels so helpless inside. The pain of the memories tears her heart out.
She's been holding it all in for so many years. Is it possible someone will hear? The tears, the fears, and all the pain. She's trying to let out. But not sure how. Isn't it safer to keep on holding it all in? Like she has been doing for all these years?
How come now she feels the need to release all these feelings? Why can't she just go on living? With the tears, with the fears, and with the pain? Why now the tears does she cry. Why now the pain does she feel? Is it because that lil girl is dying inside?
Why can't she go on crying the tears? Why can't she go on feeling the pain? And why can't she go on living with the shame? Why must she need to be released from all these things? Because this lil girl is dying inside.
http://www.angelfire.com/ok2/tellnow/index.html
Wednesday, September 12, 2007
Kids Eight Rules
1. Before I go anywhere, I always check first with my parents or the person in charge. I tell them where I am going, how I will get there, who will be going with me, and when I'll be back.
2. I check first for permission from my parents before getting into a car or leaving with anyone - even someone I know. I check first before changing plans or accepting money, gifts, or drugs without my parents' knowledge.
3. It is safer for me to be with other people when going places or playing outside. I always use the "buddy system."
4. I say NO if someone tries to touch me in ways that make me feel frightened, uncomfortable, or confused. Then I go and tell a grown-up I trust, what happened.
5. I know it is not my fault if someone touches me in a way that is not O.K. I don't have to keep secrets about those touches.
6. I trust my feelings and talk to grown-ups about problems that are too big for me to handle on my own. A lot of people care about me and will listen and believe me. I am not alone.
7. It is never too late to ask for help. I can keep asking until I get the help I need.
8. I am a special person, and I deserve to feel safe.
My rules are:
• CHECK FIRST
• USE THE "BUDDY SYSTEM"
• SAY NO, THEN GO AND TELL
• LISTEN TO MY FEELINGS, AND TALK WITH GROWN-UPS I TRUST, ABOUT MY PROBLEMS AND CONCERNS.
Copyright © 1990 National Center for Missing and Exploited Children
Monday, September 10, 2007
How Trauma Affects Children & the Benefits of EMDR Processing
In her book Children in a Violent Society Joy Osofky describes trauma as, “An
exceptional experience in which powerful and dangerous stimulus overwhelms the
infant/child’s capacity to regulate his affects”. How a child reacts emotionally to a
situation may vary greatly, depending on the context of the trauma and their living
environment: Did the child feel helpless or think his life was at risk? Did the child have a
secure or insecure attachment with the caregiver? Was a family member, friend or pet
involved? Was the child comforted and made to feel safe afterwards by her caregiver?
How often was trauma experienced, once or multiple times? At what age and stage of
development was the child at the time of the trauma? Does the child have a history of
other upsetting events or losses?
Dr. Peter Levine has described the effects of trauma in his book called Waking the Tiger
as untransformed energy which has become fixated within the organism. “Traumatic
symptoms stem from the frozen residue of energy that has not been resolved and
discharged. This residue remains trapped in the nervous system where it can wreak
havoc on our bodies and spirits.” If resolution has not occurred, the brain and the body
store the information within the neural networks and at the cellular level where it is
constantly available to be re-experienced. For children, the meaning they ascribe to an
event is what determines whether the event was traumatizing for them or not. When
parents or caregivers are not available or able to comfort a child because of their own
needs/trauma, often the trauma is reinforced, locking it into the psyche and physical body
of the child.
Unfortunately, trauma can compromise all areas of child development: identity
formation, experience of body integrity, affect tolerance, ability to manage behaviors,
cognitive processing, ability to trust self and others and spiritual and moral development.
Following trauma, the child can easily become overwhelmed and develop emotional
behavioral or physical problems which are problematic. Often not recognized in children,
PTSD symptoms develop largely because of the child’s attempts to block feeling the
negative emotions. These symptoms may show up as avoidance, dissociation and
numbing, or impulsive and/or aggressive acting out. Because these symptoms are
frequently repeated they become debilitating, self perpetuating, and accumulate over time
affecting all areas of the child’s development.
http://www.energyconnectiontherapies.com/articles/How.Trauma.Affects.Children.and.How.EMDRHelps.pdf
Saturday, September 8, 2007
Music for the soul
http://healingptsdandchildtrauma.wordpress.com/
Post-Traumatic Stress Disorder
Post-traumatic stress disorder (PTSD) is a debilitating condition that affects people who have been exposed to a major traumatic event. PTSD is characterized by upsetting memories or thoughts of the ordeal, "blunting" of emotions, increased arousal, and sometimes severe personality changes.
Description
Once called "shell shock" or battle fatigue, PTSD is most well known as a problem of war veterans returning from the battlefield. However, it can affect anyone who has experienced a traumatic event, such as rape, robbery, a natural disaster, or a serious accident. A diagnosis of a serious disease can trigger PTSD in some people. Considered to be one of a group of conditions known as "anxiety disorders," it can affect people of all ages who have experienced severe trauma. Children who have experienced severe trauma, such as war, a natural disaster, sexual or physical abuse, or the death of a parent, are also prone to PTSD.
Causes and symptoms
PTSD is a response to a profoundly disturbing event. It isn't clear why some people develop PTSD following a trauma and others do not, although experts suspect it may be influenced both by the severity of the event, by the person's personality and genetic makeup, and by whether or not the trauma was expected. As the individual struggles to cope with life after the event, ordinary events or situations reminiscent of the trauma often trigger frightening and vivid memories or "flashbacks." Symptoms usually begin within three months of the trauma, although sometimes PTSD doesn't develop until years after the initial trauma occurred. Once the symptoms begin, they may fade away again within six months. Others suffer with the symptoms for far longer and in some cases, the problem may become chronic. Some untreated Vietnam veterans with PTSD, for example, spent decades living alone in rural areas of the country, struggling to come to grips with the horror of war.
Among the most troubling symptoms of PTSD are flashbacks, which can be triggered by sounds, smells, feelings, or images. During a flashback, the person relives the traumatic event and may completely lose touch with reality, suffering through the trauma for minutes or hours at a time, believing that it is actually happening all over again
A variety of other symptoms may arise following the traumatic event. Sleep disorders such as nightmares or night terrors, or difficulty falling asleep may occur. Intense distress may be experienced when exposed to events that are associated with the trauma. Avoidance of thoughts surrounding the trauma or inability to remember the event and the accompanying emotions may also arise. Loss of interest in former pleasures (psychic numbing or blunting) or a sense of a shortened future may also be present. Startle reactions (hyper-alertness and strong reactions to unexpected noises), memory and concentration problems, moodiness, and violence may also be symptomatic. Children with PTSD may experience learning disabilities and memory or attention problems. They may become more dependent, anxious, or even self-abusing. Major depression, anxiety disorders, substance abuse, adjustment disorder, development of hypochondria disorders, and organic brain disorders may be some of the psychiatric manifestations of exposure to traumatic stress. Recovery may be slowed by injuries, damage to property, loss of employment, or other major problems in the community due to disaster.
Diagnosis
Not every person who experiences a traumatic event will experience PTSD. A mental health professional will diagnose the condition if the symptoms of stress last for more than a month after a traumatic event. While a formal diagnosis of PTSD is made only in the wake of a severe trauma, it is possible to have a mild PTSD-like reaction following less severe stress.
Treatment
Several factors have been shown to be important in the treatment of post-traumatic stress. These include proximity of the treatment to the site of the event, immediate intervention of therapy as soon as possible, and the expectation that the individual will eventually return to more normal functions. The most helpful treatment appears to be a combination of medication along with supportive and cognitive-behavioral therapies.Medications
Medications used to reduce the symptoms of PTSD include anxiety-reducing medications and antidepressants, especially the selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine (Prozac). Sleep problems can be lessened with brief treatment with an anti-anxiety drug, such as a benzodiazepine like alprazolam (Xanax), but long-term usage can lead to disturbing side effects, such as increased anger, drug tolerance, dependency, and abuse.Therapy
Several types of therapy may be useful and they are often combined in a multi-faceted approach to understand and treat this condition.
Psychological debriefing may be used as facts are recounted. Impressions, thoughts, and emotions are expressed. These responses are then validated and confirmed to be normal in response to an abnormal situation. The therapist conducting the debriefing may recommend coping skills.
Psychotherapy can help reduce negative thought patterns and self talk. This can be done on an individual basis or in groups with other PTSD sufferers. Family therapy can also be helpful.
Cognitive-behavioral therapy focuses on changing specific actions and thoughts.
Spiritual healing may also be employed and has been useful in some cases.
Alternative treatment
Several means of alternative treatment may be helpful in combination with conventional therapy for reduction of the symptoms of post-traumatic stress disorder. These include relaxation training, breathing techniques, spiritual treatment, and drama therapy, in which the event is re-enacted.
Prognosis
The severity of the illness depends in part on whether the trauma was unexpected, the severity of the trauma, how chronic the trauma was (such as for victims of sexual abuse), and the person's inherent personality and genetic make-up. With appropriate medication, emotional support, and counseling, most people show significant improvement. However, prolonged exposure to severe trauma, such as experienced by victims of prolonged physical or sexual abuse and survivors of the Holocaust, may cause permanent psychological scars.
Prevention
More studies are needed to determine if PTSD can actually be prevented. Some measures that have been explored include controlling exposure to traumatic events through safety and security measures, psychological preparation for individuals who will be exposed to traumatic events (i.e. policemen, paramedics, soldiers), stress inoculation training (rehearsal of the event with small doses of the stressful situation), and psychological debriefing.
http://www.answers.com/topic/posttraumatic-stress-disorder?cat=health
Friday, September 7, 2007
Mind & Brain / Memory, Emotions, & Decisions
Stress and Your Brain
War, rape, sexual abuse, and other severe trauma--even a car accident--could make part of your brain disappearby Robert Sapolsky
Naturally, the idea that trauma could cause a brain to shrink could be completely wrong, the sort of chicken-and-egg mess that often trips up scientists just when they think they’ve found a clue. Put a bunch of soldiers through some unspeakable hell of combat and typically only a subset of them, 15 to 30 percent, get PTSD. Maybe we have the story backward. Maybe the person with a small hippocampus who goes into a trauma is the one vulnerable to PTSD. Maybe that person processes information differently, forms memories differently, and is more at risk for flashbacks. Pitman and his colleagues have reported that soldiers who wind up with PTSD were likely to have had a higher-than-average rate of what are called “soft” neurological signs—not out-and-out neurological diseases but some minor red flags such as delayed developmental landmarks or a higher than average rate of learning disorders.
Some researchers are trying to figure out whether a small hippocampus predisposes someone to PTSD. Pitman, Arieh Shalev, and their colleagues are doing a prospective study, examining MRIs of people who have just undergone a trauma and following up with later scans. The neuroscientists will examine the before-and-after images to see whether a small hippocampus really does precede and predict who will get PTSD, or if hippocampal volume decreases in the later picture.
Meanwhile, Thomas Freeman, a psychiatrist at the North Little Rock Veterans Administration Medical Center, is taking another approach to untangling the question of cause and effect. If the hippocampus shrinks after the trauma, especially if it does so as a function of the ongoing post-trauma period, the extent of atrophy should be more dramatic in survivors of older disasters than of recent ones. Freeman and his colleagues are comparing brain scans of PTSD victims from the Gulf War, Vietnam, Korea, and so on.
So we’ve got scientists disagreeing, experiments to be done, grants to be written. What does all this mean? Let’s start with what it doesn’t mean. At present, there isn’t a shred of evidence to link everyday stress—traffic jams, money worries, crummy bosses, unhappy relationships—to neurons keeling over dead. Those stressors are not good for things like blood pressure and may result in hippocampal neurons not functioning at their best, but the neurons almost certainly remain intact. The National Institute of Mental Health defines post-traumatic stress disorder as “an extremely debilitating condition that can occur after exposure to a terrifying event or ordeal, in which grave physical harm occurred or was threatened.”
At least 4 percent of adults in the United States (5.7 million people) suffer from PTSD every year. One million Vietnam veterans have developed the disorder, as have nearly one in three people who have spent time in war zones.
Triggers include military combat, violent personal assault (rape, torture, physical or sexual abuse), accidents (car wrecks, plane crashes), natural disasters (floods, hurricanes, earthquakes). Families of victims can also develop PTSD.
http://discovermagazine.com/1999/mar/stress/article_view?b_start:int=1&-C=
Playing Games with Painful Memories:Designing VR Exposure Therapy Simulations for PTSD
Virtual Reality Exposure Therapy is currently being examined in several contexts as a treatment for post-traumatic stress disorders. Going through therapy for PTSD is decidedly not a game, and exposure therapy typically involves highly structured graded exposure treatment therapy protocols. The Virtual World Designers, for whom worldbuilding is usually much more of an art than a science, need some research and therapy savvy design guidelines. This paper explores a few ideas in this vein, drawing from the PTSD therapy literature, video game development technology, and virtual reality theory. In particular one concept originally from the field of robotics, Masahiro Mori’s Uncanny Valley, is extended in its possible application as a useful metaphor for designing virtual environments for PTSD Exposure therapy.
Ari Hollander
http://seriousgamessource.com/features/feature_053006_ptsd.php
Thursday, September 6, 2007
In-Processing
They wanted us to sweat off the juice of our identities
We stood bewildered as our past loves dripped, rolled and poured into the sand
Memories, however stuck to the tent flaps and the television and the radio and the plastic food
What we had been would stay
We naively believed that the sand and dirt that clung to our bodies that night
could be washed off...forgotten...
It transformed us, it made us all desert creatures
Stay or leave, live or die, in pain or happiness;
The heat, the sand, the desert owns us now,
And we yearn for it, and watch for it, in little houses at night...alone...
And our memories; embedded in the tents
and the televisions and the radios and
the plastic food are packed away in connex boxes
and wait for us somewhere in the Green Zone in the heart of Baghdad...
We must begin again...
-- By Sylvia Blackwood
The War Inside
Army Spec. Jeans Cruz helped capture Saddam Hussein. When he came home to the Bronx, important people called him a war hero and promised to help him start a new life. The mayor of New York, officials of his parents' home town in Puerto Rico, the borough president and other local dignitaries honored him with plaques and silk parade sashes. They handed him their business cards and urged him to phone.
But a "black shadow" had followed Cruz home from Iraq, he confided to an Army counselor. He was hounded by recurring images of how war really was for him: not the triumphant scene of Hussein in handcuffs, but visions of dead Iraqi children.
http://www.washingtonpost.com/wp-dyn/content/article/2007/06/16/AR2007061600866.html?hpid=topnews
Survivors Can Thrive!
http://survivorscanthrive.blogspot.com/
Blog Carnival
Soliders and Stress
A tremendous cost
The specialists predict the trickle of affected soldiers from Iraq now coming into clinics will turn into a flood, with serious consequences for strained Veterans Affairs budgets and for taxpayers who foot disability bills.
"We hear about the thousands of injuries -- brain injuries, leg injuries, arm injuries -- but rarely do we hear about the psychological casualties in war," said PTSD expert Dr. Evan Kanter, a neuroscientist and staff psychiatrist at the Veterans Affairs Puget Sound Health Care System in Seattle
"There will be tens of thousands of these, and the cost of that will be tremendous."
An Army survey published in the New England Journal of Medicine on July 1 said 15.6 percent to 17.1 percent of returning soldiers from Iraq exhibited signs of anxiety, major depression or other mental health problems. A new study of 1,300 Fort Bragg paratroopers who took part in the Iraq invasion echoed the findings, showing 17.4 percent exhibited PTSD symptoms.
http://seattlepi.nwsource.com/local/188143_ptsd27.html
The unseen cost of war
But PTSD specialists say reservists and National Guard soldiers appear particularly vulnerable. War is not the full-time job of the estimated 160,000 "weekend warriors" now in Iraq -- civilian soldiers who have been called up in the largest numbers since World War II. They have off-duty lives, careers and demands back home that increase stress.
http://seattlepi.nwsource.com/local/188143_ptsd27.html
Wednesday, September 5, 2007
What Are Common Signs In Adults Of Early Trauma?
What Are Some Of The Signs Older Children Exhibit After Experiencing Trauma?
coordination and balance problems
gait problems
toilet training challenges
speech delays
learning disabilities
tantrums
inappropriate aggression/timidity
depression
nightmares
response out of proportion to stimulus
inability to make eye contact
inability to ask for help
rage toward parent(s) or others
hypersensitivity
health challenges like asthma and seizures
harmful behavior towards siblings
tactile defensiveness (desire to not be touched)
http://www.beba.org/intro/trauma.php
What Are Some Known Causes Of Early Trauma?
Stressful or abusive relationship between parents during pregnancy or after birth
Maternal stress, fear or depression during pregnancy or infancy
Child was not wanted for some part of pregnancy
Considered or attempted abortion
Biochemical stresses during pregnancy from nicotine, alcohol, pesticides, etc.
Twin lost during pregnancy including early pregnancy or during birth
Chemical induction of labor
Fetal monitors that are screwed into fetus' skull
Premature birth
NICU experience with all accompanying medical interventions
Unusually long or unusually fast labor.
Being stuck during labor
Cord tightly wrapped around the neck
Near death experience or deprivation of oxygen
Medical interventions such as C-section, forceps, vacuum extraction
Anesthesia which breaks the contact between mom and baby
Separation from the mother after birth or for extended periods during infancy
Painful medical interventions such as heal sticks, spinal taps, etc.
Maternal postpartum depression or strong anxiety
Being given up for adoption
Death in the family
Unresolved traumatic history in parents or ancestors, such as early abuse, loss of a parent, traumatic birth, or being given up for adoption
Hospitalization or surgery as an infant, including circumcision
Any particularly painful accident, injury or illness
http://www.beba.org/intro/trauma.php
Why Is It Important To Heal Early Trauma?
http://www.beba.org/intro/trauma.php
What Is Early Trauma?
It has long been known that nicotine, alcohol, drug use and poor nutrition have traumatic effects on prenates and babies. We are learning that stressful family events, emotional tension and the way routine medical procedures are performed may also have long-lasting traumatic effects. In fact, trauma occurs in many different situations. It can come from something as obvious as being born prematurely or something as subtle as losing a twin in the early stages of fetal development. Early prenatal experiences like a death in the family and not being wanted are significant examples. Likewise, being whisked away from one's parents right after birth can be particularly traumatic, as can interventions like induced labor and birth by caesarian section.The term "birth trauma" specifically refers to adverse experiences one has during birth, but any traumatic events that take place between conception and about the age of three have particular significance in shaping an individual's life.
http://www.beba.org/intro/trauma.php
Sunday, September 2, 2007
Free PTSD book Open For The Love of Jack His War My Battle
Free PTSD book Open For The Love of Jack His War My Battle
http://www.members.aol.com/numbedbynumbers/for_love_of_jack.pdf
Saturday, September 1, 2007
Screaming In An Empty Room
Think PTSD numbers are bad now? Wait, they'll get worse
I've been talking about this for the last twenty five years and they are now just figuring this one out?
This is an awesome blog please check it out. Soldiers are dying because their ptsd needs are not being met.
This is a quote from the her blog "PTSD knows you are a human who feels pain in the walls of your soul."
Another quote "The thunder in your mind can turn to peace again. You can feel safe again. Talk to others in your boots until the ghosts go away.
http://namguardianangel.blogspot.com/2007/09/think-ptsd-numbers-are-bad-now-wait.html
How traumatized children perform in educational settings and why
Many traumatized children fail in school, and failure can take many forms. Children can externalize their difficulties in emotions/behaviors and find themselves in constant trouble and the subject of behavioral restrictions. Extreme examples of this are children who attempt to get expelled from school thus eliminating the problem of having to face the many challenges of going to school. Some children sit quietly and can dissociate (day dream) in the classroom and not learn. An extreme example of the internalizing child is the one who pretends to be ill, doesn’t come to school, or when they are old enough drops out of school altogether. There are many impacts of trauma that often block a child’s ability to learn in the classroom.
Trauma produces hypervigilence in children. This is a survival skill to the child in a setting where basic needs are not provided, but it is not a functional skill in school. Hypervigilence is often viewed as distractibility. In part this is due to the child focusing on aspects of the environment that are not part of the learning plan. The child in science class who is watching the non-verbal messages of a larger boy, wondering about safety during the coming recess break, is not hearing the science lesson.
Trauma produces serious self-regulation deficiencies. Often viewed as the most pervasive result of trauma, the lack of self-regulation causes these children not to have the inner understanding, inner strength, or desire to monitor emotional and behavior reactivity to events around them. This is often observed as intense emotional expression due to challenges in the classroom.
http://scarjaspermountain.wordpress.com/2007/08/31/optimum-learning-environments-for-traumatized-children%e2%80%94how-abused-children-learn-best-in-school/
Optimum Learning Environments for Traumatized Children—How Abused Children Learn Best in School
Handicapping conditions that are observable such as blindness, physical disability, deafness, autism, and even dyslexia are much better understood in educational settings than emotional disturbances and learning disabilities that come from trauma in the child’s life. For these children the answer is often a referral to the school counselor for the emotional issues that cannot be addressed in class. But this separation of the emotional and the academic challenges faced by traumatized children is not getting the job done. A child cannot compartmentalize emotions, thoughts, and behaviors as some adults can. The whole child comes into the classroom and either succeeds or fails based upon whether all aspects are engaged in the learning process rather than impeding it.
http://scarjaspermountain.wordpress.com/2007/08/31/optimum-learning-environments-for-traumatized-children%e2%80%94how-abused-children-learn-best-in-school/
Monday, August 27, 2007
Post Traumatic Stress Disorder Research
Urine Testing
Reveals low levels of cortisol which "suggests a physiological adaptation of the hypothalamic-pituitary-adrenal axis to chronic stress."
J Nerv Ment Dis 1990 Jun;178(6):366-
Low urinary cortisol excretion in Holocaust survivors with posttraumatic stress disorder compared to Holocaust survivors without ptsd. Personally I had a difficult time imagining a survivor of the Holocaust without PTSD.
"...low cortisol levels may persist for decades following exposure to trauma among individuals with chronic PTSD."
Am J Psychiatry. 1996 Jun;153(6):846.
"Increased 24-hour urinary cortisol excretion in patients with post-traumatic stress disorder and patients with major depression, but not in patients with fibromyalgia."
Acta Psychiatr Scand 1998 Oct;98(4):328-35
The results of our study suggest that initial cortisol levels in the immediate aftermath of a traumatic event contribute, in part, to subsequent symptoms of posttraumatic stress disorder.
Biol Psychiatry 2000 Nov 1;48(9):940-7
Behavioral Therapy
CBT: Cognitive Behavior Therapy
Open-label trial of cognitive behavior therapy for insomnia and disturbing dreams in crime victims with PTSD. There was significantly greater improvement.
Am J Psychiatry 2001 Dec;158(12):2043-7
Cognitive-behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Both forms of therapy were provided and they were equally very helpful in reducing anxiety and depression in the PTSD refugees.
Behav Res Ther 2001 Oct;39(10):1183-97
Virtual Reality Exposure Therapy for Vietnam Vets
Virtual reality exposure therapy for Vietnam veterans with posttraumatic stress disorder. Study revealed this form of therapy is very successful in treating Vietnam veterans.
J Clin Psychiatry 2001 Aug;62(8):617-22
Imagery Rehearsal Therapy
"Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: a randomized controlled trial... Imagery rehearsal therapy is a brief, well-tolerated treatment that appears to decrease chronic nightmares, improve sleep quality, and decrease PTSD symptom severity."
JAMA. 2001 Aug 1;286(5):584-8.
EMDR
Eye movement desensitization and reprocessing (EMDR): a meta-analysis.
This article reveals that EMDR was evaluated in 34 studies and it was found to be an effective treatment for non-combat PTSD but it no more effective than other exposure techniques "and evidence suggests that the eye movements integral to the treatment, and to its name, are unnecessary."
J Consult Clin Psychol 2001 Apr;69(2):305-16
Drug Therapy
Efficacy and safety of paroxetine treatment for chronic PTSD: a fixed-dose, placebo-controlled study.
"Doses of 20 and 40 mg/day of paroxetine are effective and well tolerated in the treatment of adults with chronic PTSD."
Am J Psychiatry 2001 Dec;158(12):1982-8
Efficacy of sertraline in preventing relapse of posttraumatic stress disorder: results of a 28-week double-blind, placebo-controlled study.
The study showed that sertraline did provide protection against relapse and provided evidence of improvement in PTSD symptoms.
Am J Psychiatry. 2001 Dec;158(12):1974-81.
Topiramate in posttraumatic stress disorder: preliminary clinical observations.
Topiramate was tested on 3 PTSD patients and it reduced and even eliminated "trauma-related intrusive memories and nightmares and normalizing depressed mood" in these patients. The study says that further study of this anti-epileptic medication for PTSD is warrented.
J Clin Psychiatry 2001;62 Suppl 17:60-3
Chemical Dependency
"An estimated 30% to 50% of cocaine-dependent individuals meet criteria for lifetime PTSD."
J Subst Abuse Treat 2001 Jul;21(1):35-45
More to Come!
http://www.mhsanctuary.com/ptsd/research.htm
Pace: Psychological Wounds Need Same Attention As Physical Wounds
“The program has done a lot for me and my family,” said a Marine veteran of the second battle for Fallujah. “I didn’t believe there was anything wrong with me when I came back to Kaneohe Baby. By the time I did, I didn’t want to do anything because of the stigma attached.”
Stigma….. that’s been a battle for the Troops who find themselves having difficulty coping with day to day life, due to PTSD. For so many years, our Troops have been told to “suck it up” and led to believe that if they sought psychological help, that they would be ostracized by their peers, or in some way punished. That stigma is something that the Department of Defense and the branches of the Military are fighting hard to overcome. They’re working non-stop to let servicemembers know that it’s alright to ask for help and by doing so, it won’t mean the end of their career. One active duty soldier involved in the program went to Camp Zama, Japan following an especially tough tour for him in Baghdad. He says that he spiraled very quickly, began abusing alcohol and continually making mistakes.
“I just didn’t care anymore,” he said. “I had hit rock bottom and I didn’t like to think about what could have happened.”
http://soldiersmind.com/2007/08/21/pace-psychological-wounds-need-same-attention-as-physical-wounds/

http://www.windyweb.com/stop.htm